FAQ Genetic conditions
Our genetic material, or DNA, is organised into 46 packages called chromosomes. Large changes that cause gains or losses of whole chromosomes are referred to as chromosomal conditions. The most common chromosomal cause of intellectual disability in children and adults is Down syndrome (trisomy 21).
No. Some conditions are caused by a genetic change within the egg or sperm for the first time without being present in either parent. These are called sporadic conditions.
Sometimes the changes causing chromosomal or genetic conditions are present in the DNA of one or both parents and can be passed on to a baby via the egg or sperm. When a change is passed on to a baby by a parent, the condition is said to be inherited.
The principle of screening is to offer a safe, accessible test to identify women with an increased chance of having a baby affected by a chromosomal or genetic condition. Women with an increased chance are offered genetic counselling and follow up diagnostic testing with amniocentesis or CVS. It is very important to understand that a screening test does not tell you for certain if your baby has the condition, only if there is an increased chance. Screening tests may also miss some babies that have the condition. Your doctor or midwife should explain the results of your screening test to you and refer you to a genetic counsellor if required.
The most common chromosomal cause of birth defects and intellectual disability in children and adults is Down syndrome (trisomy 21). Down syndrome has been the major focus of prenatal screening because it is common (occurs in about 1 in 400 pregnancies) and because it has effects on health and learning. Other chromosomal conditions that are commonly screened for include Edwards syndrome (trisomy 18) and
Patau syndrome (trisomy 13). Trisomy 18 and trisomy 13 are more severe conditions than Down Syndrome and are associated with a high rate of pregnancy loss or death in infancy. For more information, see the resources below.
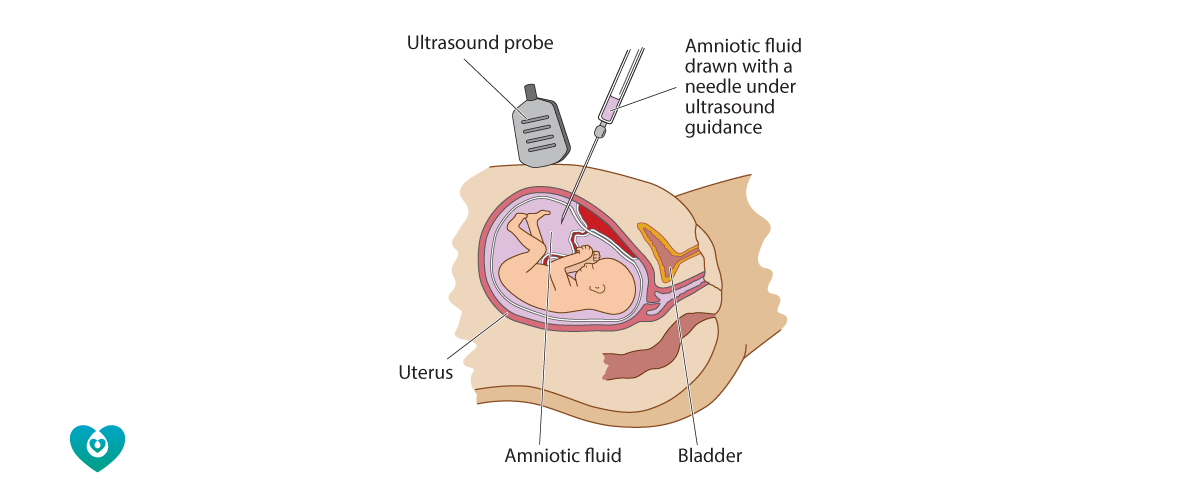
An amniocentesis is a medical procedure that samples a small amount of the fluid from around the baby using a needle inserted through the woman’s abdomen. The most common reason for having an amniocentesis is to check the health of the baby. Women may choose to have an amniocentesis if there is a concern that the baby may have Down syndrome or another chromosome condition. This concern could be due to an abnormal finding on ultrasound, or due to a result of a prior screening test. Sometimes a woman may have an amniocentesis to test the baby for other conditions such as an inherited disease or an infection.
Amniocentesis is not recommended before 15 weeks gestation. Your doctor should fully explain the reasons for offering an amniocentesis to you and obtain your written consent before performing the procedure.
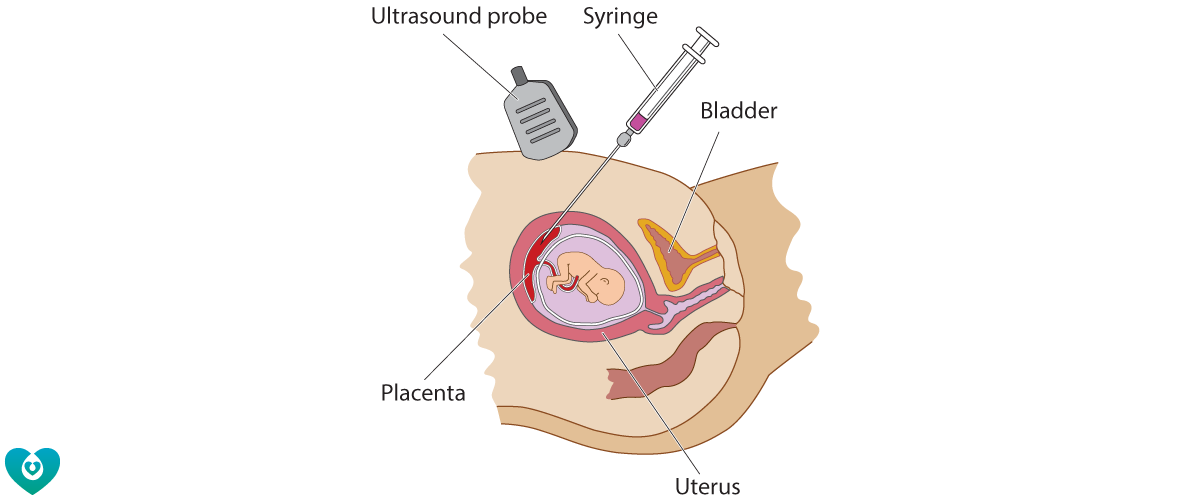
A CVS (chorionic villus sampling) is a medical procedure performed to sample cells from the placenta during pregnancy. It is usually done with a needle inserted through the woman’s abdomen (transabdominal CVS). Less commonly, a CVS can be performed through the vagina and the neck of the womb (transcervical CVS). The most common reason for having a CVS is for diagnostic testing for Down syndrome or another genetic condition in the pregnancy. A CVS can be performed earlier in pregnancy than amniocentesis (from 11 weeks, compared with 15 weeks for amniocentesis).
There is a small risk that an amniocentesis or CVS may cause a miscarriage. In general, the risk of miscarriage due to a complication from amniocentesis or CVS is less than 1 in 200 (0.5%).
In order to minimise complications, an amniocentesis should not be performed before 15 weeks, and a CVS should not be performed before 11 weeks. Your doctor should also know your blood group and your hepatitis B, hepatitis C and HIV status before performing any invasive procedure during pregnancy.